
Brain injury is an ancient affliction. In fact, primitive peoples, and even early humans experienced traumatic head trauma and recognized the repercussions of such injuries. Ancient Greeks understood that the brain was the center of cognition, and that a blow to the head could disrupt memory, thinking, and even emotional response.
Over the course of human history, healers, shamans, and primitive surgeons understood the devasting effects of brain injury, that an injured brain could cripple the body, change personality, and alter the human psyche. In fact, evidence of trepanation, an archaic form of brain surgery in which burr holes were drilled into the skull to relieve pressure from neurologic or psychic injury, has been found in skulls dating back to the Neolithic period. This practice was believed to cure, or at least treat the consequences of brain injury, and it was practiced, in some form, until the 19th century.
Today, brain trauma is considered a public health crisis, affecting 1.7 million Americans each year. Approximately 1.4 million sufferers are treated at emergency rooms, while 275,000 are hospitalized and 52,000 die from TBI. The impact of brain trauma is far reaching: Though TBI can happen to anyone, such injuries disproportionately afflict the young and productive, causing death, disability, and long-term psychological damage.
Heightened public awareness of brain injury has focused on the danger of sports related concussions and post-concussive syndrome, a condition that may increase risk for a variety of neurologic and psychiatric outcomes. However, brain trauma includes a broad and complex constellation of neurologic and psychiatric symptoms, and a diagnosis of Traumatic Brain Injury (TBI) can be a far reaching one that impacts an individual’s life for months or years.
But just what is a traumatic brain injury, and how has modern medicine shed light on this ancient affliction; mapped the cascade of psychiatric and neurologic trauma that can follow? And how have advances in modern neuroscience informed litigation, especially of those diagnosed with ensuing psychiatric maladies that so often come with a blow to the head?

The Spectrum of Brain Injury
Brain injury has historically been associated with war time injuries in soldiers but is now recognized as a cause of debilitating cognitive and psychological impairment in the general population. And although traumatic brain injury has come to be associated with concussions in athletes, statistics show that such injuries increasingly result from falls, motor vehicle accidents, assaults, and other blows to the head.
The CDC defines a traumatic brain injury “as a disruption in the normal function of the brain that can be caused by a bump, blow, or jolt to the head, or a penetrating head injury.” Any injury that causes displacement of the brain within the skull can lead to a TBI.
The three levels of traumatic brain injury – mild, moderate, and severe – are each defined by the presence and/or degree of loss of consciousness, confusion, physical, and/or cognitive/behavioral changes. While moderate and severe head injuries are the most serious and potentially life threatening, most traumatic brain injuries that occur each year are mild (MTBI) and are marked by a brief (or nonexistent) loss of consciousness and some transient signs of confusion, disorientation, or amnesia. However, patients diagnosed with MTBI exhibit a range of symptoms, from a fleeting headache to a 30-minute period of unconsciousness. Because of the heterogeneity of symptoms, as well as a lack of biomarkers, or precise diagnostic tools with which to determine the level of brain injury, MTBI can be difficult to classify and diagnose with precision. In fact, there is no consensus among professional medical organizations regarding the criteria for diagnosis of MTBI.
This diagnostic conundrum is illustrated by confusion around MTBI and concussion, terms that have been used interchangeably by many practitioners, even though experts disagree on whether these are two distinct conditions. No matter what the diagnostic label, however, research shows that even a mild head injury can be far more insidious than previously thought.
And so, the need to discover, to decipher the still cryptic brain, its capacity to endure trauma and depression, is ongoing, a series of trials and errors, a journey that originated long before our time.
Axons: The Brain’s Fiber Optics
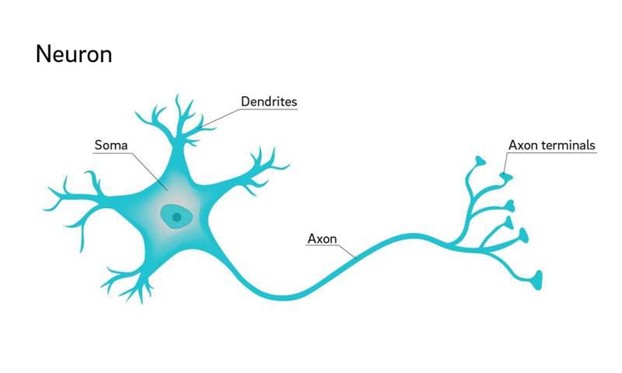
The human brain is a complex configuration of white and gray matter; it is comprised of 100 billion neurons that communicate with each other and signal information to all regions of the body. Each neuron is composed of a cell body, an axon, and a dendrite. Neuron bodies, or soma, which contain the nucleus, are formed in bundle like tracts and make up the brain’s gray matter. Gray matter is arranged around the outer perimeter of the brain and comprises 40 percent of total brain volume.
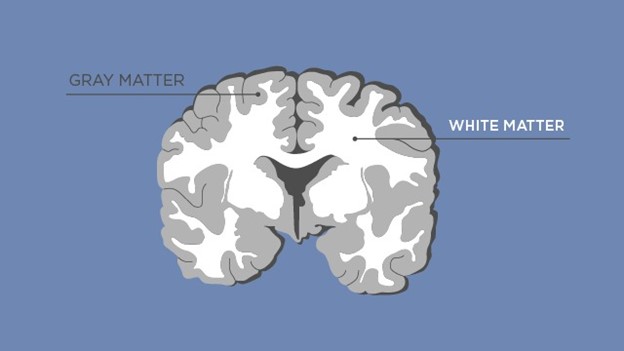
Axons are the long filament like attachments that extend from each neuron; they are arranged in clusters, and connect to, and make up white matter, which comprises 60 per cent of the brain. White matter, through its axons, allows communication to and from both gray matter and other parts of the body.
Axons range from 1,000 to 10,000 times the length of the cell body of each neuron. The diameter of an axon is microscopic, perhaps one micrometer across, but some, like that of the sciatic nerve which travels from the spine to the tip of the big toe, are elongated. Axons serve as transmitters of electrical signals that the soma, or neuron body use to communicate. They are elegant instigators of information between neurons. Movement, touch, even the process of thinking, are all inspired by the relay of signals from neuron to neuron, by the chemical and electrical impulses running like lit wires along the axons, traveling to destinations within the human body.
When head injury is sustained, nerve fiber, or axons, are stretched and sheared, and this disruption of brain tissue is believed to be the crux of many traumatic brain injuries. Changes in white matter, in the neurons and axons imbedded in it, are thought to be related to brain diseases such dementia and stroke. Ongoing research on TBI continues to reveal that similar white matter changes may be responsible for the persistent debilitating symptoms of some brain injured patients. Some of these symptoms, such as memory changes, emotional instability, and depression are similar to those of white matter disease. In fact, research around head injury suggests that damage to white matter is in some way linked to many degenerative brain processes.
From the study of axons, we also know that brain trauma is not a static event, one that begins and ends with an initial blow to the head. In fact, medical literature describes TBI as a cascade of events that transpire over the course of hours and days. The initial injury triggers a series of metabolic, biochemical, and inflammatory processes that continue to alter the brain’s functioning for weeks, or even months. MTBI patients who have prolonged symptoms of cognitive dysfunction and emotional instability beyond three months duration are diagnosed with post-concussion syndrome, a disease which may result from the continuing course of axonal injury.
Mild TBI, once thought to be self-limited and benign, has been linked to more serious forms of progressive brain disease such as Parkinson’s and Alzheimer’s Disease, especially in those who have sustained multiple head injuries.
Diffusion Tensor Imaging and TBI
Severe complications resulting from traumatic brain injury, including skull fracture, brain edema, and intracranial hemorrhage, can be seen with conventional imaging modalities such as CT scan and MRI. These types of injuries are more often seen with moderate or severe TBI. In patients who have a mild TBI, only 10% of CT scans and 30% of MR scans show subdural or subarachnoidal hemorrhage.
However, the pathophysiology of brain injury, especially mild TBI, is often not visible, even upon sophisticated imaging. That is because conventional MRI and CT scans detect structural defects which may not be present in MTBI, or are below the threshold of their imaging capacity. The subtle changes, damage to the axons, seen in all levels of TBI, is not detected on MRI or CT scans.
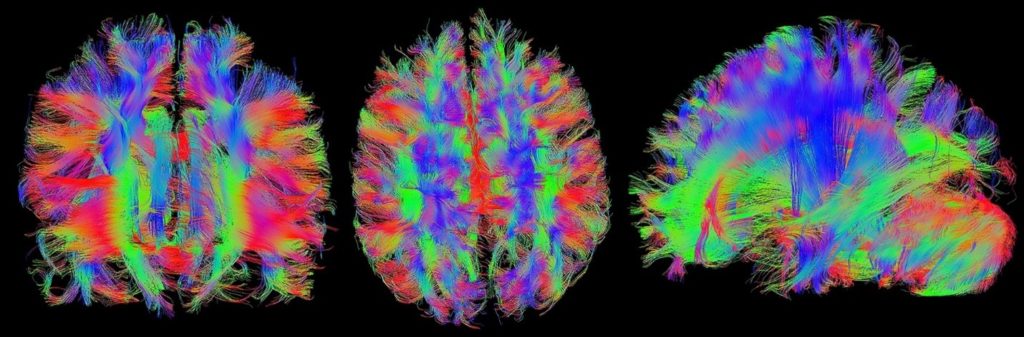
Newer imaging technologies, such as diffusion tensor imaging, or DTI, however, capture more specific information about the injured brain than conventional MRI technology, and can suggest possible white matter abnormalities.
This is especially important in cases of MTBI because microscopic axonal injury is not detected with conventional imaging studies. Such unrecognized damage to white matter increases the risks of long-term functional impairment. DTI is useful for understanding the pathophysiology of mild TBI by detecting and analyzing hidden axonal disruption that would not otherwise be visualized.
DTI is an advanced MRI technique that was first used in 2002 to investigate mild TBI. This form of imaging takes advantage of the fact that the human body, including white matter, is composed mostly of water. DTI measures how far water molecules move within the very structured region of white matter. Studies have shown that, in patients with brain injury, there is a disordered movement of water. In fact, it has been shown that patients with mild TBI have changes in white matter that correlates with the reduced cognition seen in brain injured patients.
Both legal experts and medical professionals seek more definitive ways to visualize and diagnose TBI, and DTI appears to objectify changes specific to brain trauma in a way that MRI and CT scans do not, potentially allowing for a more precise diagnosis. Because DTI imaging does indeed reveal changes in white matter that suggest an injury or disease process in MTBI, it has been heralded as an exciting new technology with the potential to eventually diagnose and prognosticate on brain injured patients.
Still, there are multiple concerns about the application of DTI to brain injury diagnosis. DTI imaging reveals patterns of white matter damage, but the cause of such damage in individual patients is nonspecific. In fact, there are many causes of white matter changes seen in DTI imaging. Are such changes due to brain injury, or to another pathological process, an inborn error, or the result of an aging brain? Furthermore, DTI does not show a picture of definitive white matter injury in the way that an x-ray reveals a bone fracture: Instead, it displays altered patterns of water diffusion across tracts of white matter, a finding which requires a series of inferences in determining the actual reason for such changes.
DTI has primarily been used in research settings to study groups of patients afflicted with TBI, and there is no standard applied to the many studies using this technology. It is, therefore, difficult to apply this imaging technique to individual diagnoses with the necessary degree of accuracy.
In fact, diffusion tensor imaging is not yet a standard part of the diagnostic and treatment protocol for TBI for this reason nor is it presently recommended for this purpose.
The Illuminated Brain: The Emergence of Psychoradiology
Like brain trauma, depression has been recognized throughout human history as a malady, one that plagues the mind and spirit. Early writings from Mesopotamia reflect on depression as a spiritual affliction, one that required the intervention of a priest, or asipu. It was thought that demons or bad spirits might be forced out of the body using rituals and incantations. A millenium later, Ancient Greeks described depression as melancholia, a distinct disease thought to derive from an imbalance of the bodily humors. By the 11th century, Persian physician Avicenna laid out the basis of modern medicine with The Canon of Medicine, a work that stood alongside the writings of Hippocrates and Galen. Avicenna’s early theories on depression provide a foundation for contemporary ideas about mental illness.
Today, the Diagnostic and Statistical Manual of Psychiatric Disorders, the authoritative text used by mental health professionals to diagnose and define mental disorders, categorizes depression as a “mood disorder that causes a persistent feeling of sadness and loss of interest.” Although the DSM 5 also outlines specific criteria necessary for the diagnosis of major depression, this diagnosis remains a subjective one. Loss of appetite, a feelings of worthlessness, and a diminished ability to work or think, for example, are possible symptoms of major depression.
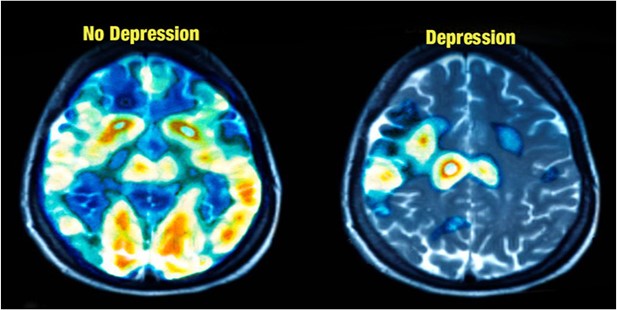
Modern theories of depression cut lines across history, from the purely psychodynamic models of the early 19th century, to the more recent view of depression as an organic disease. Advances in imaging technologies, though, have, allowed for an intimate view of the depressed brain, one that reveals structural and functional changes that might one day provide biomarkers for mental illness. The emerging field of psychoradiology applies imaging technology to the discipline of psychiatry, allowing for a shift in the definition of depression and other mental illnesses away from strictly psychological constructs toward the realm of brain disorder.
Attempts to map the depressed brain are challenging, though. Depression has a complex and heterogenous constellation of symptoms that represent multiple subtypes. Physicians rely on clinical symptoms to diagnose a disease that is configured by many unknowns: The physiology of the brain and its intricate connections to the endocrine system, individual genetics, and emotional factors are not fully understood, and hinder a full understanding of major depression.
Researchers in the nascent field of psychoradiology analyze these subtypes to find brain images that correlate with each type. Another investigational method is to image and analyze the brain while the patient is engaged in task-based activities, as cognitive and emotional triggers can highlight patterns of depression.
MRI imaging also shows that people with depression have less activity in the prefrontal cortex, an area of the brain that helps to regulate emotion.
Although psychoradiology is a young discipline, one that is still limited to investigation and research, continuing advances in radiologic imaging may one day allow this field to bring necessary biomarkers to the diagnosis and care of depressed patients.
And though much has been learned about the depressed brain over the past twenty years, the etiology of this ancient affliction remains controversial, a riddle, secreted by human history. Although we can illuminate its corridors with modern imaging techniques, the hidden workings of the brain, and its synergy with genetics, physiology, human emotion, environmental factors, and trauma are still elusive.
The Interface Between Depression and MTBI
Psychiatric disturbances are frequent long-term outcomes of TBI. PTSD, anxiety, sleep disorders, and depression are all possible sequelae of TBI. Major depression occurs in at least 40% of individuals in the year following a TBI. Cohort studies of TBI patients show that some individuals do not become depressed, while others are transiently or persistently afflicted. Depression, however, is by far the most common psychiatric outcome of TBI and is associated with poorer long-term outcomes in mild TBI patients.
Earlier theories of post head injury depression and psychiatric illness centered on “accident neurosis,” which discounted possible physiologic factors that might contribute to ongoing symptoms.
And still, the relationship between TBI and mood disorders is not completely understood. Why does depression occur so frequently after a blow to the head? Psychological and emotional factors surely come into play in some cases. Afterall, the stress of dealing with the repercussions of TBI cannot be minimized. And so, it is difficult to parse these subtle factors from the biological changes and disruptions that are at play in the traumatized brain.
And although clinical depression is an independent diagnosis with defined risk factors and a constellation of symptoms, this mood disorder frequently occurs in individuals who have an existing medical condition. Those who suffer from MS, heart disease, lupus, and diabetes, for example, frequently develop a coexisting depression. In fact, chronic illness can trigger depression in some patients. But which came first, the preexisting condition, or the depression; and how might one instigate the other?
Although the Diagnostic and Statistical Manual of Mental Disorders (DSMV), classifies such co-existing depression as depressive disorder due to another medical condition, the question of causation remains unanswered.
Is the connection between TBI and depression clearer, though? Are there factors that suggest a head injury instigates depression in some physiologic manner – in a way that is not yet determined in other cases of disease and comorbid depression?
One prospective study showed that depression was far more common in a group of TBI patients than in a control group of individuals who suffered orthopedic trauma. Although both groups suffered trauma, only the head injured patients developed depression in the post injury period. This and similar findings suggest that structural or functional changes in the traumatized brain, and not emotional trauma, prompt depression in TBI patients. These changes are reflected in neuropsychological testing or by abnormal neuroimaging studies in some patient cohorts.
DTI imaging, which has revealed unique changes in the traumatized brain, has also been used to decipher the differences between post-concussion patients who are depressed, and those who are not. One such study, reported in the Radiological Society of North America, finds that depressed concussion victims have decreased functioning of white matter similar to that of non-traumatic major depression sufferers. Another report, from Frontiers in Neurology Neurotrauma, shows that people with TBI have increased brain connectivity between multiple regions of the brain and the amygdala, that part of the brain which processes emotion.
These studies and others suggest that affective disorders are a consequence of brain trauma, perhaps sheared axons that disrupt the interaction between prefrontal regions that process emotions and mood regulate mood. A significant number of these patients will develop ongoing or persistent depression that is not possible to predict.
Still, questions about post TBI depression, sometimes subsumed under a diagnosis of post concussive syndrome, remain. Although studies have shown a correlation between head injury and depression, it is not clear if this relationship is causative or if post TBI depression is sometimes a psychological coping mechanism. It is also true that a history of pre-injury depression or mental health diagnoses increases risk of post-concussive symptoms. Some TBI patients, for example, have pre-existing depression that resurfaces after a TBI.
Can ongoing research in brain injured patients reveal, in the near term, insights into the connection between TBI and depression, or are such studies only a beginning, a view toward the links that connect us to pain, to trauma, to the long human history of depression that has followed us?
The Birth of Neurolaw

Because brain injury complications can be disabling, MTBI patients sometimes seek legal counsel to secure disability, to protect their rights in the workplace, or to win damages in a negligence case. Some brain traumatized patients undergo personality changes and develop new impulsive behaviors, behaviors that put them at risk for criminal activity or drug seeking. Many suffer from life-altering major depression that persists long after the original head injury was sustained. Consequences of head injury are often not seen on imaging, or able to be diagnosed by conventional studies.
Historically, it has been challenging for brain injured plaintiffs to show that their “invisible” injuries are real and not simply fraudulent claims brought for secondary gain because the court system relies on tangible proof of harm. Many outcomes of TBI are emotional, psychiatric, or not definitively correlated to the original injury. Courts have been unwilling to award damages under such circumstances.
Tort law, which deals with civil matters, rests on the foundation of physical evidence to show damages. Unlike broken bones and fractures, which are clearly discernible, depression, anxiety, and other outcomes of head injury are not readily evidenced. Implicit in this argument is the theory of “substance dualism”, a deeply rooted societal belief that holds that emotional harm is less deserving of compensation than physical injury.
In addition, emotional or mental harm has been much more difficult to prove because neuroscience has not had the capacity to diagnose and verify such injuries. Advances in neuroimaging have allowed a more sophisticated view of the relationship between the brain and psychological changes and suggests the possibility of eventual parity in the treatment of physical and emotional pain.
The emerging field of neurolaw attempts to bridge the gap between brain science and litigation around those impacted by debilitating head injury or neuropsychiatric disease by applying the latest innovations in neuroscience to such cases. For example, brain imaging technology such as DTI might show that a plaintiff has marked changes in white matter that are associated with depression or other psychiatric diagnoses. Such findings could bolster the plaintiff’s case when seeking damages due to a head injury.
Innovative imaging technologies may also be used in criminal cases to either mitigate a defendant’s culpability or bolster the prosecution, depending on the medical findings.
Early use of imaging technology was introduced by John Hinkley’s defense team in 1981. Hinckley, who attempted to assassinate President Ronald Reagan, was found not guilty by reason of insanity, in part because his lawyers introduced Hinckley’s CT scan as evidence that he had an atrophied brain. This atrophy, the defense claimed, was evidence of schizophrenia, a diagnosis that could support an insanity defense. Experts countered that brain atrophy was not evidence of schizophrenia, merely that such atrophy was more common in schizophrenic patients.
Though neuroimaging has become much more sophisticated since the 1980’s, its limitations remain. Just as John Hinckley’s CT scan could not prove that atrophy caused his schitzophrenia, DTI imaging cannot show causation between white matter disruption and events that may have provoked it. It has been primarily used to find patterns of brain signal data consistent with groups of individuals who have sustained brain injury.
Even when abnormalities in white matter are detected, it is difficult to discern the cause of these lesions because there are many other possible diagnoses. Recent studies show that some people with psychiatric symptoms have the same pattern of white matter alteration as brain injured individuals.
Because of the concerns around the diagnostic and clinical application of DTI, many academic medical organizations have cautioned about its use in these contexts. The American Society for Functional Neuroradiology has issued a suggested disclaimer on clinical use of DTI, which states that “it is critical that physicians basing clinical decisions on DTI be familiar with the limitations and potential pitfalls inherent to this technique.” A multidisciplinary conference to address the “use and abuse” of neuroimaging, hosted by the American College of Radiology in 2012, stated that “the neuroradiology community has not arrived at a consensus view of the value of DTI in…head trauma.”
More recently, a Radiological Society of North America guideline statement issued in 2018 urged caution in the interpretation of DTI at the individual level.
Despite concerns from medical societies, as well as some legal experts, courts are trending toward admissibility of DTI to diagnose TBI in civil cases. Recent evidence of this change is reflected in a civil case from a Superior Court of Washington, in which the Court upheld the admissibility of DTI imaging. The Court found that plaintiff’s experts were not relying primarily on TBI imaging to render a diagnosis of TBI. This is an important part of the Court’s decision, as the medical literature reflects on the importance of bolstering DTI imaging with other types of testing that also supports a diagnosis of TBI.
Advocates of neurolaw hope that the introduction of such technology in the courtroom will lead to a deeper understanding of the brain, shifting the way that the law understands and interprets human behavior, cognition, and emotion from a restrictive or punitive approach to one that is more equitable. In the context of civil law, such an understanding might allow brain injured individuals who have suffered unrealized trauma and psychiatric disability to be recognized as victims of legitimate harm and to be compensated for it.
But will neurolaw transform the courts, especially in the arena of tort law, which has historically defined harm as a consequence of physical injury?
And would such a shift truly advance the cause of mentally and emotionally injured people in the near term? Will the application of sophisticated new technologies rescind what many believe to be outmoded thinking about mind-body dualism and its place in the courtroom?
Although the law seems to be at a tipping point, as the courts increasingly allow DTI to be admitted in TBI cases, many questions remain about the veracity of imaging technology, and DTI in particular, as a means to diagnose mental pain, illness, and anguish as a consequence of head injury.
Lawsuits involving TBI have nearly tripled over the past two decades, and the need for courts to understand the complexities behind TBI cases is more important than ever. However, the admission of DTI into the courtroom does not necessarily clarify the question of head injury causation, or the relationship between TBI and depression in individual civil cases.
Instead, jurors are left to ponder the complexities of this imaging from information distilled through opposing expert witnesses. Yet questions persist around DTI’s suitability for TBI diagnosis, questions that experts in neuroimaging and brain science continue to grapple with.
Advances in neuroscience allow for a nuanced and sophisticated understanding of the human brain. Emerging legal disciplines and subspecialties of medicine, such as neurolaw and psychoradiology are evolving; forging new and profound ways to understand behavior, to see and treat the traumatized brain.
But will the application of new technologies be tempered by insight, by an understanding that each advance is an incomplete vision of a bigger scheme, one that flickers and moves further from our line of sight with each discovery? And that knowledge, the history of brain trauma itself, is elusive, still sequestered in human memory, in the delicate fibers that we seek to illuminate?


 Heffernan Research offers a range of English language tutoring options. Individual and small group sessions are available. Special classes on focused topics, such as essay writing, are also offered throughout the year. Margot works with ESL students as well as individuals who need to enhance specific English language skills.
Heffernan Research offers a range of English language tutoring options. Individual and small group sessions are available. Special classes on focused topics, such as essay writing, are also offered throughout the year. Margot works with ESL students as well as individuals who need to enhance specific English language skills.
 Margot Heffernan has solid and extensive experience writing about a broad range of medical topics. She uses her expertise to provide comprehensive and academically sound papers for medical malpractice, product liability, and personal injury lawyers as well as other professionals who need reliable medical information.
Margot Heffernan has solid and extensive experience writing about a broad range of medical topics. She uses her expertise to provide comprehensive and academically sound papers for medical malpractice, product liability, and personal injury lawyers as well as other professionals who need reliable medical information.